|
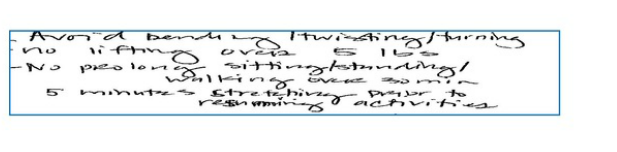
First doctor, part of the carrier’s Medical Provider Network, said:”Back to work in no time after a small surgery.” The other doctor, chosen by the injured worker’s lawyer, opined that the worker cannot even seat more than 30 minutes as inscribed below: Workers Compensation Insurance law is set up to protect the well beings of injured workers and also to mitigate the liability exposure of the employers in case a worker is injured in the course of work. After a worker got injured at the course of work, the worker is protected from being terminated from his or her position even he or she cannot perform the duty anymore. Also the employer cannot force the injured to undergo treatment that is selected by the employer.
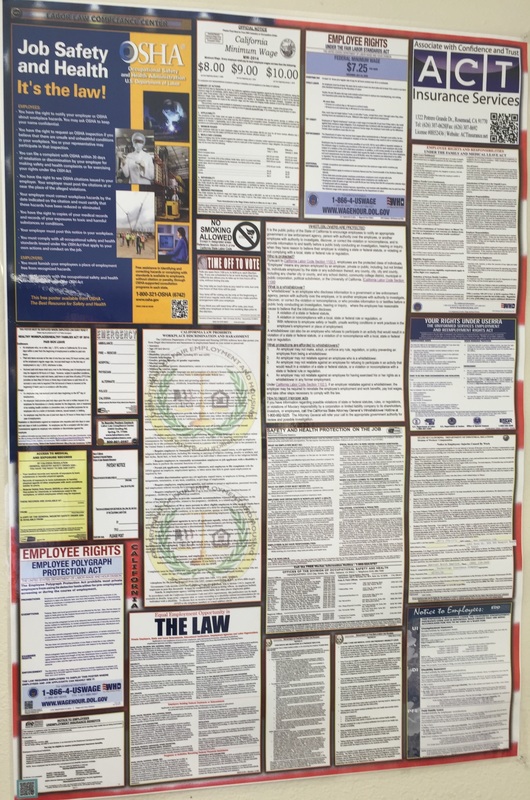
The above scenario apparently brings forward a loss/loss situation to the employer. What can the employer do then? To answer the above question, let’s go back to 2004 when Governor Arnold signed the SB 899 into law that strongly suggested the WC carriers or employers to set up a Medical Provider Network after Jan 1, 2005. If an employer or insurer uses an approved Medical Provider Network, covered employees would receive their medical carrier in this network, unless a predestined physician is chosen prior to an injury. Then forward to Sept. 18, 2012 when Governor Brown signed SB 863 into law that took effective on Jan 1, 2013, another milestone Workers Compensation Law of California. Let’s get into the new regulations regarding Medical Provider Network: Treatment obtained from a non-network provider, without either authorization from the employer or insurance carrier or a workers’ compensation judge’s order permitting outside of network treatment, will not have to be paid for by the employer or carrier. If unauthorized treatment is unsuccessful, and results in a worsening of the injured worker’s condition, or a need for additional treatment, the employer/carrier will have no obligation to pay for that, either. Now back to the loss/loss scenario that the employer is confronting. The first doctor is belonging to the MPN (Medical Provider Network) chosen by the carrier/employer and the second doctor is referred by the lawyer that the injured worked sustained and he is a “non-network provider”. According to SB 863, the carrier would not validate the second diagnosis and either the employer or the carrier would be responsible for the treatment payment. Is the employer stuck in the Limbo? Not quite, the WC carrier would be the party best suited to handle the case. Just sit tight and let the carrier’s claim adjuster to deal with the conflicting diagnoses and the WC claim. The carrier understands the law, they have the expertise and that is what they deal with everyday. This is probably the most important reason but always unaware by the insured why they should buy insurance: to transfer the litigation burden to the carrier who is obliged to defend the insured if the claim is falling under the covered causes of loss. The litigation cost could easily be ballooned into hundreds of thousands of dollars even the claim may be proved to be baseless. For those who are interested to know more about the newest WC law, click on the following link to review the overview of SB863 as prepared by the Department of Industrial Relations. http://www.dir.ca.gov/dwc/Reports/SB863-Assessment-WC-Reforms-July-2015.pdf For the employers, please post the poster that outlined the most updated labor law where your employees can easily see. Posting the poster is required by law and would help you to mitigate the claim against you when there is a work related injury. Check out the MPN information; accident happens and it would save valuable time if you know where to send the injured worker when accident does happen. For the employees, information on the poster is vital for you to know your rights and where to get help if you feel that your rights are violated.
1 Comment
|
AuthorSteve Yuen Archives
November 2021
Categories |
Copyright 2018 ACT Insurance Services, Inc - License# 0H52436 | [email protected]

 RSS Feed
RSS Feed